 Injury survivors from racial and ethnic minority groups experienced greater improvements than White injury survivors in their posttraumatic stress disorder (PTSD) symptoms after receiving a stepped collaborative care intervention. This was the finding of a secondary analysis of data from the Trauma Survivors Outcomes and Support (TSOS) study, an NIH Pragmatic Trials Collaboratory Trial led by principal investigator Doug Zatzick of the University of Washington.
Injury survivors from racial and ethnic minority groups experienced greater improvements than White injury survivors in their posttraumatic stress disorder (PTSD) symptoms after receiving a stepped collaborative care intervention. This was the finding of a secondary analysis of data from the Trauma Survivors Outcomes and Support (TSOS) study, an NIH Pragmatic Trials Collaboratory Trial led by principal investigator Doug Zatzick of the University of Washington.
The report was published online in Trauma Surgery & Acute Care Open.
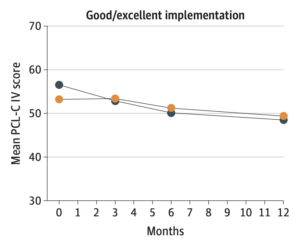
In the TSOS study's main analysis, which was published in JAMA Surgery in 2021, the researchers saw a significant reduction in PTSD symptoms at 6 months in the intervention group compared with the control group. In the new secondary analysis, they saw that reduction in symptoms among racial and ethnic minority patients but not among White, non-Hispanic patients.
The findings "suggest that the previously reported 6-month treatment effects derive predominantly from intervention-related PTSD symptom improvements in non-white/Hispanic patients," wrote author Khadija Abu and colleagues from the University of Washington and the University of California, Los Angeles.
The TSOS study, an NIH Collaboratory Trial, was a stepped-wedge, cluster randomized pragmatic clinical trial testing the delivery of a stepped collaborative care intervention vs usual care for injured patients with PTSD symptoms and comorbid conditions. The study was conducted at 25 level I trauma centers in the United States. Of the 635 patients in the trial, 350 were from racial backgrounds other than White—including 218 patients who identified as African American, 15 as American Indian or Alaska Native, 8 as Asian or Pacific Islander, and 109 as multiple or other races. One-hundred two patients were Hispanic.
Patients in the control group received usual care plus nurse notification about their high level of distress. Patients in the intervention group received collaborative care consisting of evidence-based medication, cognitive behavioral therapy, and case management.
The study team proposed a few possible explanations for their findings:
- In addition to its universal components, the TSOS intervention and referral elements consisted of tailored components designed to address the needs of a multicultural patient population by incorporating social determinants of health.
- Collaborative care models include shared decision-making approaches, which are thought to enhance patients' engagement in care in racial and ethnic minority populations and other underserved groups.
- In the year before their injury, almost half of the white, non-Hispanic patients in the study had accessed mental health services, compared with only about a quarter of the non-White and Hispanic patients, suggesting that participation in the study improved access to mental health care for patients in racial and ethnic minority groups.
A commentary accompanying the article praised the TSOS research team for "taking important steps to care for adverse sequelae associated with traumatic injury," and noted that "these first steps represent giant leaps for health equity" for underserved populations.
The TSOS study was supported within the NIH Pragmatic Trials Collaboratory by a cooperative agreement from the National Institute of Mental Health and by the NIH Common Fund through a cooperative agreement from the Office of Strategic Coordination within the Office of the NIH Director. Learn more about the NIH Collaboratory Trials.



 The
The 
 NIH Collaboratory researchers in 2021 shared study results, generated new knowledge, and developed innovative research methods in pragmatic clinical trials. Their work included insights from the Coordinating Center and
NIH Collaboratory researchers in 2021 shared study results, generated new knowledge, and developed innovative research methods in pragmatic clinical trials. Their work included insights from the Coordinating Center and 

 NIH Collaboratory researchers in 2020 reported study results, generated new knowledge, and developed innovative research methods in pragmatic clinical trials. Their work included insights from the Coordinating Center and
NIH Collaboratory researchers in 2020 reported study results, generated new knowledge, and developed innovative research methods in pragmatic clinical trials. Their work included insights from the Coordinating Center and  A recent article in Ethics & Human Research describes the experience and management of regulatory noncompliance during the conduct of a large, multisite embedded pragmatic clinical trial (ePCT). The
A recent article in Ethics & Human Research describes the experience and management of regulatory noncompliance during the conduct of a large, multisite embedded pragmatic clinical trial (ePCT). The