
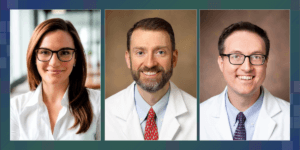
In this Friday’s PCT Grand Rounds, Ken Mahaffey of Stanford University and Nishant Shah and Neha Pagidipati of Duke University will present “CardioHealth Alliance: A Platform to Improve Care.”
The Grand Rounds session will be held on Friday, May 17, 2024, at 1:00 pm eastern.
Mahaffey is the associate dean for clinical research in the Stanford University School of Medicine and the director of the Stanford Center for Clinical Research. Shah is an assistant professor of medicine in the Duke University School of Medicine and the principal investigator for the REVEAL Project: Identifying Real World Gaps and Areas for Improvement. Pagidipati is an associate professor of medicine in the Duke University School of Medicine and the principal investigator for the Test to Treat: Improving Lipid Management on a Health System Level.









 In this Friday’s PCT Grand Rounds, Michael Pencina of Duke University will present
In this Friday’s PCT Grand Rounds, Michael Pencina of Duke University will present