A primary care intervention for patients with coexisting chronic kidney disease, type 2 diabetes, and hypertension did not reduce the hospitalization rate for these patients when compared to usual care, according to the ICD-Pieces study.
The results of the study were published this week in the New England Journal of Medicine.
ICD-Pieces, an NIH Collaboratory Trial, was a cluster randomized, pragmatic clinical trial testing an intervention that used an electronic health record–based algorithm and practice facilitators in 141 primary care practices. The study team randomly assigned more than 11,000 adults to receive either the intervention or usual care. The large, diverse study population—of whom 20% were Black and almost 20% were Hispanic or Latino—was representative of the population with chronic kidney disease, type 2 diabetes, and hypertension in the United States.
In the intervention group, the study team used an algorithm to identify patients in the electronic health record in real time. Practice facilitators then worked with the participating primary care providers and patients to meet blood pressure targets, promote use of appropriate medications, achieve goals for blood glucose control, and engage in other guideline-directed care. The intervention period lasted 12 months, and the primary outcome was hospitalization for any reason.

At the end of the study, the hospitalization rate was similar between the intervention group and the usual care group. Rates of key secondary outcomes, such as emergency department visits and cardiovascular events, were also similar between the groups.
“Although we did not observe a difference in the primary outcome, we believe the study is an important step in advancing our understanding of how to conduct pragmatic trials embedded in healthcare systems,” said Dr. Miguel Vazquez, the principal investigator for ICD-Pieces and a professor of internal medicine at UT Southwestern Medical Center in Dallas.
The study team identified and enrolled a large number of patients, including a large proportion of patients who are members of racial and ethnic groups that are usually underrepresented in clinical trials, Vazquez explained. Moreover, the intervention was delivered across 4 large healthcare systems using a variety of electronic health record systems, there was fidelity in intervention delivery, and there was robust capture of outcomes in a diverse population with multiple chronic conditions.
Vazquez also emphasized the value of conducting the ICD-Pieces study as an NIH Collaboratory Trial.
“The opportunity to work within the NIH Pragmatic Trials Collaboratory was essential for the successful completion of our trial,” Vazquez said. “Access to the expertise from the Coordinating Center and ongoing interactions with investigators from other projects provided critical knowledge to conduct our study embedded in large health systems,” he added.
ICD-Pieces is supported within the NIH Pragmatic Trials Collaboratory by a cooperative agreement from the National Institute of Diabetes and Digestive and Kidney Diseases.




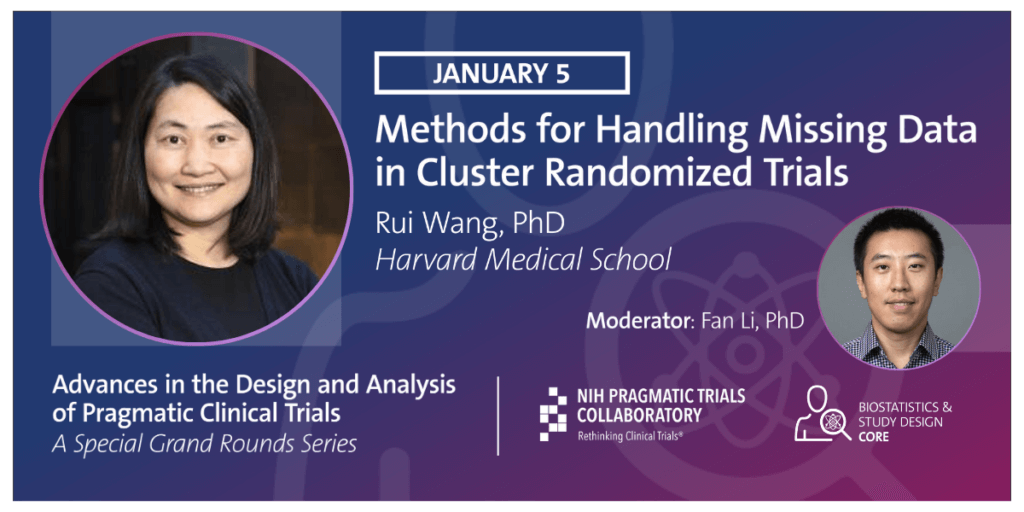 In this Friday's PCT Grand Rounds, Rui Wang of Harvard Medical School will offer the final session in our special series, Advances in the Design and Analysis of Pragmatic Clinical Trials, with
In this Friday's PCT Grand Rounds, Rui Wang of Harvard Medical School will offer the final session in our special series, Advances in the Design and Analysis of Pragmatic Clinical Trials, with  In this Friday’s PCT Grand Rounds, Jonathan Moyer of the NIH Office of Disease Prevention will continue our special series, Advances in the Design and Analysis of Pragmatic Clinical Trials, with his presentation,
In this Friday’s PCT Grand Rounds, Jonathan Moyer of the NIH Office of Disease Prevention will continue our special series, Advances in the Design and Analysis of Pragmatic Clinical Trials, with his presentation,  The NIH Pragmatic Trials Collaboratory is launching a
The NIH Pragmatic Trials Collaboratory is launching a 

 Organizational culture, clinician training and support, the ability to link patients to ongoing treatment, and the ability to tailor implementation to each clinical site were key determinants of successful implementation of an intervention to promote buprenorphine initiation in emergency departments, according to a qualitative study conducted as part of the EMBED pragmatic clinical trial.
Organizational culture, clinician training and support, the ability to link patients to ongoing treatment, and the ability to tailor implementation to each clinical site were key determinants of successful implementation of an intervention to promote buprenorphine initiation in emergency departments, according to a qualitative study conducted as part of the EMBED pragmatic clinical trial. In this Friday’s PCT Grand Rounds, Matthew Semler of Vanderbilt University will present
In this Friday’s PCT Grand Rounds, Matthew Semler of Vanderbilt University will present  In this Friday’s PCT Grand Rounds, Amit Garg and Stephanie Dixon of Western University’s Schulich School of Medicine & Dentistry will present
In this Friday’s PCT Grand Rounds, Amit Garg and Stephanie Dixon of Western University’s Schulich School of Medicine & Dentistry will present 