 In this Friday’s PCT Grand Rounds, Jim Hughes of the University of Washington will continue our special series, Advances in the Design and Analysis of Pragmatic Clinical Trials, with his presentation, “Guidelines for Design and Analysis of Stepped-Wedge Trials.” The session will be held on Friday, December 1, at 1:00 pm eastern.
In this Friday’s PCT Grand Rounds, Jim Hughes of the University of Washington will continue our special series, Advances in the Design and Analysis of Pragmatic Clinical Trials, with his presentation, “Guidelines for Design and Analysis of Stepped-Wedge Trials.” The session will be held on Friday, December 1, at 1:00 pm eastern.
Hughes is a professor emeritus of biostatistics at the University of Washington. This session’s moderator, Patrick Heagerty, is a professor of biostatistics at the University of Washington and a cochair of the NIH Pragmatic Trials Collaboratory’s Biostatistics and Study Design Core.
This special Grand Rounds series will include additional moderated webinar discussions that bring together biostatisticians, clinical trials methodologists, and investigators to discuss challenges and share lessons learned in the design, implementation, and analysis of pragmatic trials. Download the series flyer and see the full schedule below.
- October 6, 2023: Hybrid Studies Should Not Sacrifice Rigorous Methods (David M. Murray, PhD; Moderator: Jonathan Moyer, PhD)
- November 3, 2023: The Perils and Pitfalls of Complex Clustering in Pragmatic Trials (Jonathan Moyer, PhD; Moderator: Andrea Cook, PhD)
- December 1, 2023: Guidelines for Design and Analysis of Stepped-Wedge Trials (Jim Hughes, PhD; Moderator: Patrick Heagerty, PhD)
- January 5, 2023: Methods for Handling Missing Data in Cluster Randomized Trials (Rui Wang, PhD; Moderator: Fan Li, PhD)
All sessions are free and open to the public; no registration is required.



 In this Friday’s PCT Grand Rounds, David Murray of the NIH Office of Disease Prevention will kick off our special series, Advances in the Design and Analysis of Pragmatic Clinical Trials, with his presentation,
In this Friday’s PCT Grand Rounds, David Murray of the NIH Office of Disease Prevention will kick off our special series, Advances in the Design and Analysis of Pragmatic Clinical Trials, with his presentation,  The NIH Pragmatic Trials Collaboratory is launching a
The NIH Pragmatic Trials Collaboratory is launching a  In this Friday’s PCT Grand Rounds, Richelle Koopman of the University of Missouri will present
In this Friday’s PCT Grand Rounds, Richelle Koopman of the University of Missouri will present 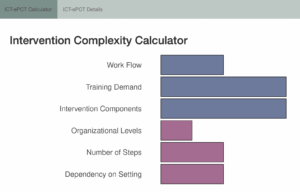

 The NIH Pragmatic Trials Collaboratory has developed an online
The NIH Pragmatic Trials Collaboratory has developed an online  This Friday’s PCT Grand Rounds will feature the next installment of our special series, Ethical & Regulatory Dimensions of Pragmatic Clinical Trials. Monica Taljaard and David Magnus will present
This Friday’s PCT Grand Rounds will feature the next installment of our special series, Ethical & Regulatory Dimensions of Pragmatic Clinical Trials. Monica Taljaard and David Magnus will present