 This year’s Annual Steering Committee Meeting for the NIH Pragmatic Trials Collaboratory featured implementation science as one of the topics of focus. In an interview after his keynote presentation, Dr. David Chambers, deputy director for implementation science at the National Cancer Institute, shared his thoughts on opportunities for implementation science in the context of pragmatic trials.
This year’s Annual Steering Committee Meeting for the NIH Pragmatic Trials Collaboratory featured implementation science as one of the topics of focus. In an interview after his keynote presentation, Dr. David Chambers, deputy director for implementation science at the National Cancer Institute, shared his thoughts on opportunities for implementation science in the context of pragmatic trials.
Why Implementation Science Is Important in Pragmatic Research
Chambers described the overlap between implementation science and pragmatic research and how this creates several benefits. Implementation science gives a heightened focus on how to get interventions to be as accessible, well used, and beneficial as possible to populations within the systems and communities in which people are seeking and receiving healthcare.
“The earlier researchers can think about their interventions being used beyond the trial, the better,” Chambers explained. “Implementation science helps to provide a lens for multiple levels of change that may be needed, including supports for patients and families, clinicians, clinics, systems, policymakers, and other key decision-makers.”
Furthermore, implementation science methods can save time in identifying barriers and facilitators for delivering interventions with high quality-knowledge which can be applied toward the ultimate use of interventions.
Chambers encourages researchers to embrace the dynamism that is reflected in our health systems, which is particularly apt for research conducted in the setting of routine care. “It is a given that there will be deviations from the design of an intervention and its implementation, so how can researchers learn from this?” he said.
In terms of sustaining an intervention, a more dynamic approach is needed to how the intervention and the context will change over time, he explained. “Too often we think of sustainment in terms of fixing things in their original state. Sustainment needs to think about how to build in evolution-medicine and our practices are evolving.”
Role of the NIH Pragmatic Trials Collaboratory
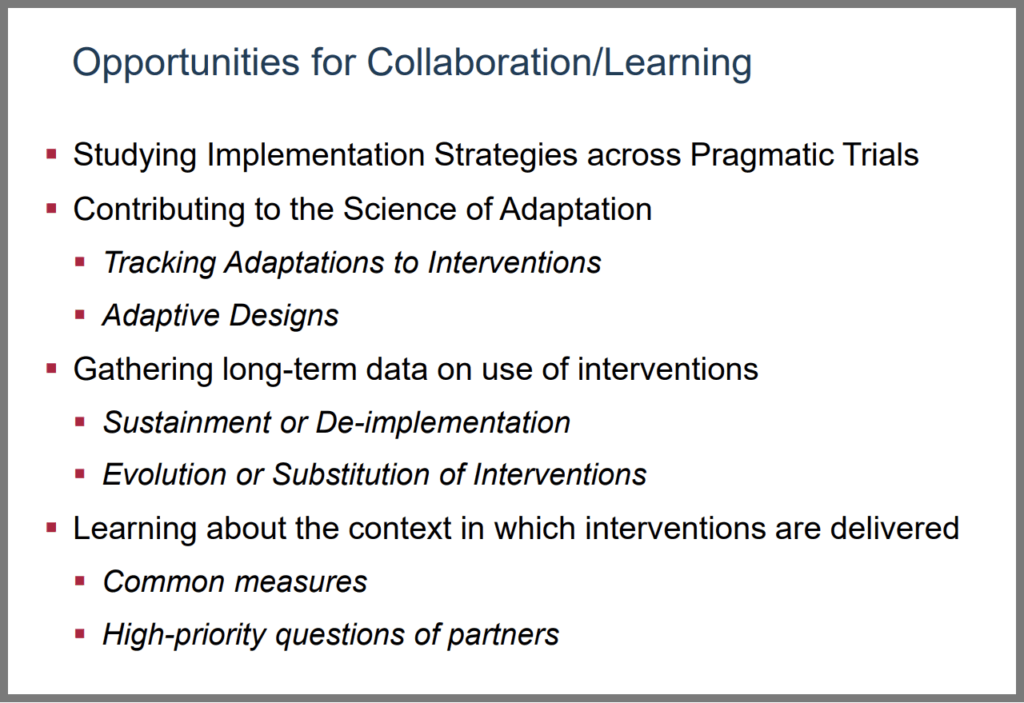 According to Chambers, the NIH Pragmatic Trials Collaboratory provides a natural setting for implementation activities because of the close partnerships between the investigative teams and the health systems and community settings where the research occurs. As a result, the program is poised for ongoing learning from the strategies health systems are using to implement a range of different interventions.
According to Chambers, the NIH Pragmatic Trials Collaboratory provides a natural setting for implementation activities because of the close partnerships between the investigative teams and the health systems and community settings where the research occurs. As a result, the program is poised for ongoing learning from the strategies health systems are using to implement a range of different interventions.
There is also an opportunity for pooling lessons across the NIH Collaboratory Trials, such as common measures that can be used to better characterize adaptation, understanding perspectives and needs of patients and clinicians, and approaches related to long-term sustainment or deimplementation of interventions.
Increasingly for NIH Collaboratory trials, issues related to implementation are baked into both the design of interventions and the approach used to test the interventions, which is a testament to the program’s ongoing progress in encouraging the use of implementation science concepts and methods.
Learn more about the NIH Collaboratory’s Implementation Science Core.
How NIH Is Advancing Implementation Science
For over 20 years, NIH has recognized the gaps in knowledge needed for successful implementation of evidence-based interventions. Across NIH institutes, centers, and offices, they have discussed the common challenges observed when investigators saw a positive result in their trial and were frustrated that it could not be replicated and scaled up in the real world.
NIH funds dissemination and implementation research grants and has a standing review panel, the Science of Implementation in Health and Healthcare, focused on this area where any applicant to NIH can suggest that their grant be reviewed. In addition, NIH supports training opportunities in the field and cohosts an annual scientific conference in partnership with AcademyHealth.
NIH continues to explore the interface between effectiveness and implementation, think about deimplementation, and work on tackling misinformation, all towards advancing how to better apply the evidence generated in research to optimize population health and healthcare.




