This year’s annual Steering Committee meeting for the NIH Pragmatic Trials Collaboratory featured 2 special guests from the US Food and Drug Administration’s Digital Health Center of Excellence—Matthew Diamond, MD, PhD, Chief Medical Officer, and Sonja Fulmer, PhD, Acting Deputy Director. They joined to share information on the FDA’s approach to clinical decision support (CDS) software, including the agency’s recently released guidance, which helped stimulate a discussion on the associated considerations for embedded pragmatic clinical trials. Here we highlight some key takeaways from that discussion.
CDS is a broad term that encompasses a range of different functions, and there are several NIH Collaboratory Trials that are testing CDS software. Diamond explained that some digital health technologies, including some CDS software, meet the regulatory definition of a medical device while others do not. The FDA focuses its oversight on a subset of digital health technologies.
The new FDA guidance outlines criteria for determining which CDS are considered non-devices due to the CDS criteria in the 21st Century Cures Act. In addition to the CDS guidance, there are other policies that may apply to a digital health technology, so the FDA created a Digital Health Policy Navigator to help people find the relevant guidance for their situation. Further, the FDA encourages engagement early and often to understand how the regulations and policies apply to a particular product or technology.
If a software is the focus of FDA’s regulatory oversight, it does not mean the research cannot be done. In fact, research is essential to contribute to the body of evidence on the functioning of a device. The research just needs to go through the right processes. The goals of using the right processes for product review and research are to ensure that patients are protected during research and that the products that are ultimately marketed are safe and effective. The determination of whether an investigational device exemption (or IDE) is required is based on risk.
The details behind the implementation of digital health products matters a lot in these determinations. Subtle differences in the way that a product functions and the claims that are made about a product can make a big difference. Diamond stressed the importance of clearly defining the intended use of a product, including who it is intended for and what the user is supposed to do with information provided by the software. Fulmer highlighted the importance of transparency with stakeholders, including healthcare professionals, patients, and regulators.
For specific questions, the presenters encouraged researchers to reach out to the FDA’s digital health experts at DigitalHealth@fda.hhs.gov.




 The US Food and Drug Administration last week issued
The US Food and Drug Administration last week issued  The US Food and Drug Administration (FDA) will
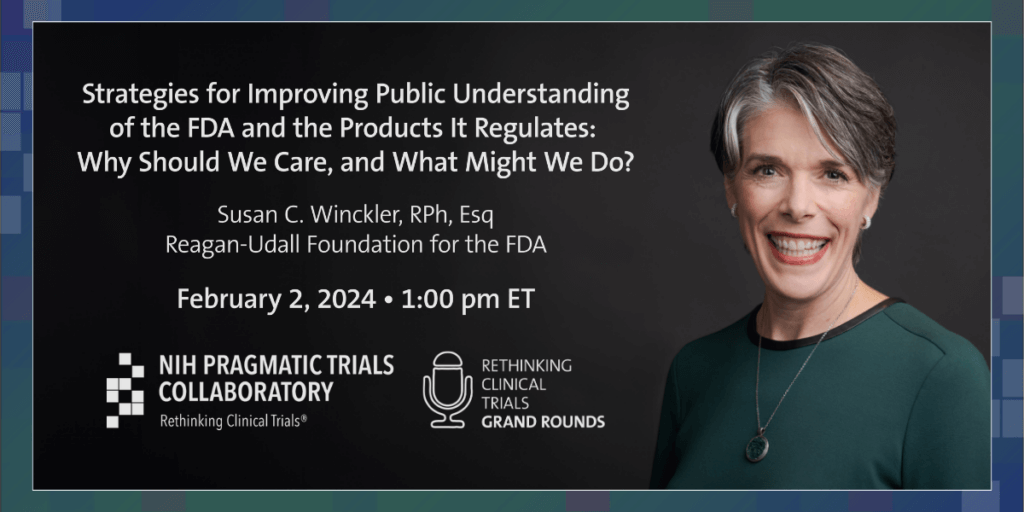
The US Food and Drug Administration (FDA) will  In the latest episode of the
In the latest episode of the