Speaker
Natalia E. Morone, MD, MS
Associate Professor of Medicine
Boston University/Boston Medical Center
Keywords
Chronic pain; Mindfulness; Stress Reduction; Low back pain; OPTIMUM; The Pain, Enjoyment of Life and General Activity (PEG) Scale; HEAL Initiative
Key Points
- Chronic back pain is very common across all racial and ethnic groups. Doctors treat chronic back pain with non-pharmacologic methods before resorting to pharmacologic treatments.
- Optimizing Pain Treatment in Medical Settings Using Mindfulness (OPTIMUM) is a randomized study of mindfulness for low back pain operating in 3 health settings: Boston Medical Center; UPMC, Pittsburgh, PA; and University of North Carolina, Chapel Hill in partnership with Piedmont Health Services.
- Participation in the OPTIMUM study requires 8 weekly 90 minute group-based sessions of mindfulness meditation training delivered in primary care through a telehealth medical visit with follow up assessments at 6 and 12 months.
- Four methods of mindfulness meditation are taught: Walking meditation, body scan, breath focused meditation, and mindful stretching.
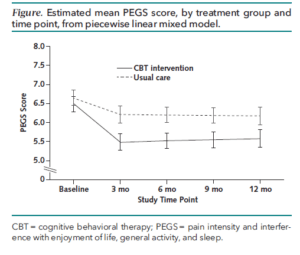
- The OPTIMUM study uses the PEG scale as the main outcome measure at the 6 and 12 month follow up assessments.
- Group tele-health visits provide a variety of benefits for patients including more time with a clinician, better medication adherence, and more patient satisfaction.
Discussion Themes
Primary care usually consists of 1 provider and 1 patient, but family medicine evolved to see patients in a group. This group setting model may have unexpected benefits.
OPTIMUM is part of the PRISM project and is collecting data on participant use of opioids along with all PRISM projects.
Recruiting minority participants has been a priority in the OPTIMUM trial. Targeting recruitment advertisements to zip codes where more minorities live makes a difference in recruiting a diverse population.
Read more about the OPTIMUM trial.
Tags
#pctGR, @Collaboratory1



 The Agency for Healthcare Research and Quality (AHRQ) published a new
The Agency for Healthcare Research and Quality (AHRQ) published a new